BRAINS IN BRIEFS
Scroll down to see new briefs about recent scientific publications by neuroscience graduate students at the University of Pennsylvania. Or search for your interests by key terms below (i.e. sleep, Alzheimer’s, autism).
Adolescent nicotine exposure fundamentally changes the brain to make subsequent morphine use in adulthood more rewarding
or technically,
Paradoxical Ventral Tegmental Area GABA Signaling Drives Enhanced Morphine Reward After Adolescent Nicotine
[See original abstract on Pubmed]
Dr. Ruthie E. Wittenberg was the lead author on this study. Ruthie is currently a postdoc in the lab of Paul Kenny at the Icahn School of Medicine at Mount Sinai. Her research is focused on the intersection of cellular immunology and addiction neuroscience. In the future, she hopes to establish an independent academic research career studying the neurobiology of substance use disorders and motivated behaviors.
or technically,
Paradoxical Ventral Tegmental Area GABA Signaling Drives Enhanced Morphine Reward After Adolescent Nicotine
[See Original Abstract on Pubmed]
Authors of the study: Ruthie E. Wittenberg, Sanghee Yun, Kechun Yang, Olivia K. Swanson, Shannon L. Wolfman, Lorianna M. Colón, Amelia J. Eisch, and John A. Dani
In the United States, drug overdose is a leading cause of death, and most drug overdoses involve the use of opioids. Opioids (sometimes called narcotics) are often medically prescribed for treating chronic pain. However, opioids, whether prescribed or not, have high abuse risk, and taking them can lead to opioid use disorder (OUD). OUD is a type of substance use disorder or addiction that involves a “problematic pattern of opioid use that causes significant impairment or distress” according to the CDC. Anyone can become addicted to opioids, but some things might make it more likely for someone to develop OUD. For example, adolescent nicotine use is a risk factor for developing OUD later in life. Most tobacco use begins during adolescence, with teens vaping or using nicotine pouches.
The link between early-life nicotine use and OUD is not well understood, so for her PhD in the labs of John Dani and Amelia Eisch, former NGG student Ruthie Wittenberg wanted to understand how nicotine use during adolescence could change the brain to promote morphine reward in adulthood.
Adolescence is the time in development when the brain is more flexible and with greater plasticity than in adulthood. One such part of the brain, the ventral tegmental area (VTA), is considered to be the start of the main reward pathway. Increased neuronal activity, altered dopamine signaling, and structural changes are examples that all contribute to increased reward sensitivity. Evidence from both human and animal studies indicate that using drugs during adolescence, when the brain is most flexible, can create long-lasting changes in the brain and in behavior that can extend into adulthood.
To understand how adolescent nicotine exposure changes reward-related behaviors in adulthood, Ruthie gave adolescent mice nicotine for 2 weeks and waited until they were older to see how they responded to opioids, like morphine. She wanted to see how adult mice who had been exposed to nicotine earlier in life responded to the rewarding properties of opioids compared to mice who had never been exposed to nicotine. Ruthie used a conditioned place preference (CPP) paradigm in mice to test reward learning. CPP works like this: there are different chambers or “contexts.” They differ in both visual and tactile cues. Each context has a different pattern of stripes or colors on the wall to help the mice be able to tell the difference between the chambers. The floor of each chamber also differs (e.g. they have distinct ridges or grooves), providing a tactile cue.
In this case, mice received morphine in one chamber, and a control drug (saline) in another chamber for 3 days. After the 3 days, Ruthie allowed the mice to move freely between the chambers and measured how much time they spent in the morphine-paired chamber compared to the saline-paired chamber. If mice spent more time in the reward chamber than the saline chamber, this indicated they were able to associate that context with the reward (the opioid), and that they remembered that this chamber felt more rewarding. Ruthie tested the mice who had been previously exposed to nicotine and mice who had never been given nicotine in the morphine CPP test, and she found that mice that had been exposed to nicotine spent more time in the morphine chamber than the group of mice that never had nicotine. The non-nicotine group still remembered the chamber where they got morphine but they spent significantly less time there than the nicotine group. In conclusion, Ruthie found that morphine was even more rewarding to the nicotine-exposed mice than the mice who were never exposed to nicotine.
Ruthie further explored what changes in the brain are happening because of adolescent nicotine use to make this behavior happen?
To understand the link between using nicotine in adolescence and morphine later in adulthood, Ruthie looked at the VTA, the origin of the reward pathway. The VTA is made up of neurons that release one or more neurotransmitters to communicate with each other. It is also well-known for producing dopamine, which motivates the seeking of drugs and other rewards. Additionally, the VTA releases other neurotransmitters, like GABA, which helps to quiet other neurons, like those that release dopamine. Since the brain is really flexible in adolescence, Ruthie wanted to know if changes in VTA GABA neurons could be a link between nicotine use in adolescence and morphine use in adulthood.
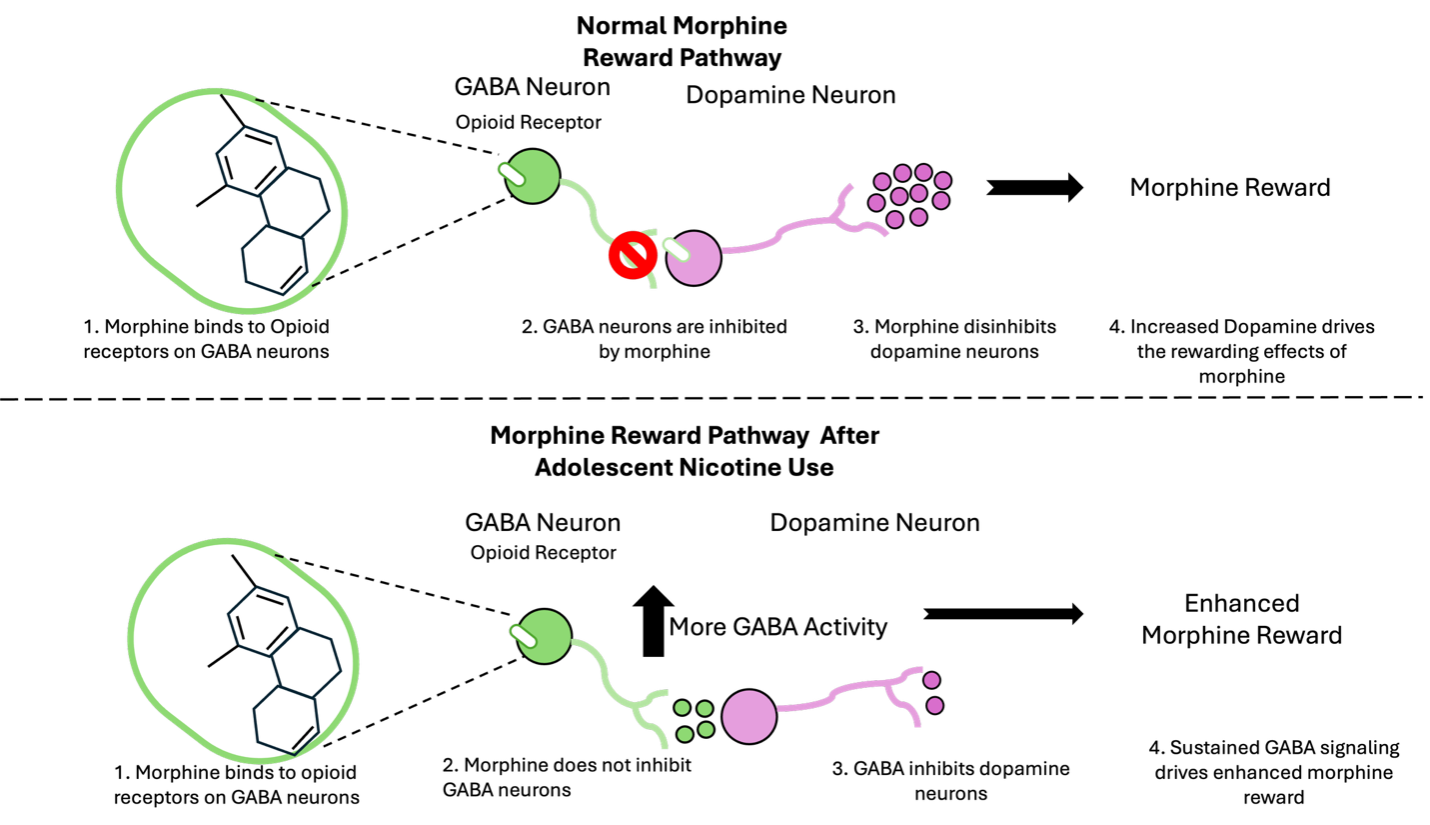
Chronically using nicotine in adolescence changes how VTA GABA neurons communicate with other neurons. Ruthie wanted to know how adolescent nicotine use changes how VTA GABA neurons respond to morphine in adulthood. As a result, she used patch-clamp electrophysiology to record the electrical activity of these neurons. An important thing to note is that opioids like morphine bind to endogenous opioid receptors, meaning receptors mice already have on their VTA GABA neurons. When morphine acts on these receptors, it inhibits neural activity. Moreover, GABA neurons quiet the VTA dopamine neurons and morphine quiets GABA neurons, allowing dopamine neurons to release more dopamine, leading to the rewarding effects of morphine. This process is called disinhibition, where the neurons that inhibit (GABA neurons) are inhibited themselves, which allows other neurons to start to fire.
Figure 1: Schematic representation of how the VTA reward circuit is fundamentally altered after adolescent nicotine use.
Ruthie found that adolescent nicotine use changed the way that this neural circuit was acting, such that morphine no longer disinhibits dopamine neurons (Figure 1). By recording from GABA and dopamine neurons in the VTA in adult mice, she found that among mice exposed to nicotine as adolescents, morphine no longer inhibited GABA neurons and it also did not change how dopamine neurons fired.
Ruthie’s results would suggest that sustained GABA neuron activity seemed to be driving the increased reward behavior seen in the CPP experiment. To test this, Ruthie artificially inhibited VTA GABA neurons in mice that had nicotine exposure during adolescence (enabling the VTA GABA cells of the nicotine animals to act like those of the water animals) and observed that the enhanced reward learning previously seen was blocked.
In conclusion, Ruthie determined that the VTA circuit is fundamentally changed after adolescent nicotine exposure. After adolescent nicotine use, VTA GABA neurons are no longer inhibited by morphine and additionally, mice find morphine more rewarding than normal. These findings challenge the canonical view of the brain’s reward system and advance our understanding of the mechanisms driving addiction-related behaviors. This may explain why prior drug exposure can make it more likely that people develop disorders like OUD. Great job Ruthie!
About the brief writer: Lucas Tittle
Lucas Tittle is a PhD Candidate in the labs of Dr. Guillaume de Lartigue and Dr. Kevin Bolding. His research is at the intersection of the olfactory system and gut-brain axis, and how external signals like odors and internal signals interact to change feeding behavior.
If you want to read more Click here!
Sex matters: Exploring sex differences in opioid withdrawal mechanisms
or technically,
Sex differences in VTA GABA transmission and plasticity during opioid withdrawal
[See original abstract on Pubmed]
Dan Kalamarides was the lead author on this study. Dan’s research interests are rooted in neuropsychopharmacology, that is, the intersection of brain physiology, drugs (both “good” and “bad”), and behavior. This interest has been applied in the context of preclinical models for several therapeutic areas including substance use disorders, pain, neuroinflammation, and depression. Dan is currently planning to transition to industry where he can leverage his neuroscience expertise in the pharmaceutical world to enhance treatment strategies for mental health disorders and brain diseases.
or technically,
Sex differences in VTA GABA transmission and plasticity during opioid withdrawal
[See Original Abstract on Pubmed]
Authors of the study: Daniel Kalamarides, Aditi Singh, Shannon Wolfmann, John Dani
Scientific research has long been biased on the basis of sex. From cells and tissues to animals and people, there is a long history of scientists including more male subjects in their studies. As a result, we don’t understand how female bodies respond differently to diseases or to treatments, and the quality of healthcare has suffered. The National Institutes of Health (NIH) and several scientific journals have started requiring researchers to consider sex in their science, but the progress towards equal representation of males and females has been slow.
Opioids - including heroin, fentanyl, morphine, and others - are one of many classes of drugs that affect men and women differently. For example, women are less responsive to the pain killing effects of opioids but more sensitive to affects the drugs have on respiration compared to men. This difference makes it a lot harder to safely and effectively treat women with opioids in the clinical setting, and it can make recreational opioid use more dangerous. Despite these differences in people, basic science research into the effects and mechanisms of opioids in females is still lacking compared to our understanding of the drugs in males.
One area of research on opioids that still has a lot of unanswered questions, related to sex differences and more generally, is opioid withdrawal. Scientists, including recent NGG graduate Daniel Kalamarides, want to better understand opioid withdrawal so that they can treat the withdrawal, help people feel better, and make it easier for people to stop using opioids. In his paper, Daniel and his fellow researchers wanted to learn more about how the brain changes during opioid withdrawal, while keeping in mind that these changes could look different in males and females. Specifically, he was curious about a brain region called the ventral tegmental area (VTA), which contains neurons responsible for releasing dopamine into another brain region (the striatum) involved in reward.
Previous studies have shown that the active effects of opioids (think the “high”) are in part caused by an increase in dopamine release from those neurons in the VTA. This happens because opioids remove a natural brake on the dopamine system. In an opioid-free brain, other inhibitory neurons in the VTA – known as GABAergic neurons because they release the neurotransmitter GABA – decrease the release of dopamine from the dopaminergic neurons. Opioids remove this brake by decreasing the activity of the inhibitory neurons. This makes the system go faster, or, more specifically, release more dopamine.
Your brain adapts if opioids are in the body for an extended period of time. In the VTA, this means that those inhibitory neurons amp up their control of the dopamine-releasing neurons so that, even in the presence of an opioid, a relatively normal amount of dopamine is released. This is fine until the opioids are removed. Now you have an overactive brake, and there’s not enough dopamine released into the reward-related brain regions.
Researchers have found, in male mice only, that the inhibitory neuron control of the dopamine-releasing neurons increases in withdrawal because the connections between them grow stronger. This increase in connectivity is known as long term potentiation (LTP) or plasticity, and it’s one of the primary mechanisms by which the brain changes depending on how it’s used and what it’s exposed to. Knowing that the effects of opioids can differ between males and females, Daniel explored whether a similar phenomenon occurs in female mice.
Daniel first induced opioid withdrawal in mice by giving them morphine for a week, then studied the properties of neurons in the VTA when the mice were in withdrawal. He used patch-clamp electrophysiology, a technique which allowed him to measure the electrical current flowing into or out of the neuron as he manipulated the voltage. By using this technique, he was able to learn about the strength of the connection between the inhibitory neurons and the dopaminergic neurons and compare that connection between male and female mice.
Daniel measured how likely the inhibitory neurons were to release GABA – and thus inhibit the dopamine-releasing neurons – spontaneously and when electrically stimulated. He found that, in male mice, morphine withdrawal increased the probability of GABA release (or increased the strength of that brake). This was a great result because previous studies had also found this phenomenon, which means that this science is replicable. When he looked at female mice, however, he didn’t see any difference between the morphine treated mice and the control mice. That’s a surprise!
Daniel also tried to experimentally force LTP to occur in the brains in morphine withdrawal so that he could learn more about how the probability of GABA release was changing. He stimulated the inhibitory neurons with a really high frequency of electrical current, which would cause LTP in a normal neuron. He found that he could cause plasticity in the female mice, but he couldn’t in the males. This result suggested that the increase in the probability of GABA release in males was due to LTP. The molecular components needed for LTP were all used up in the males, so Daniel couldn’t create more. The components were still available in the females, on the other hand, so Daniel was able to stimulate the neurons and cause LTP.
To be thorough, Daniel also asked if the male and female mice were experiencing a similar level of morphine withdrawal. If the female mice were going through less withdrawal, it could maybe explain the sex differences in plasticity in the VTA. Daniel measured the strength of withdrawal that the mice were experiencing by counting physical signs of morphine withdrawal, and he found that males and females displayed a similar number. After all of these experiments, we still don’t know for sure that the opioid withdrawal mechanisms in male and female mice are entirely different. If Daniel used a different dose of morphine or if he studied the brains at a different time into withdrawal, he might be able to observe the same plasticity in female mice that he saw in male mice. However, by running this control experiment, he was able to strengthen the argument that there is a true difference in how the male and female mouse brains changed in opioid withdrawal.
This research by Daniel and his fellow scientists reinforced the fact that opioids affect males and females differently, and they showed that we still don’t understand how female brains change in opioid withdrawal. Hopefully, this evidence will push other scientists to continue thinking about sex differences in opioid research and in neuroscience broadly. In the meantime, Daniel has led us a step closer towards developing treatments for opioid use disorder, and he’s contributed to reducing bias in science.
About the brief writer: Lyndsay Hastings
Lyndsay is a first year NGG PhD student broadly interested in the relationship between neurocircuitry and behavior.
Interested in learning more about how opioid withdrawal is different in males and females? Check out Daniel’s paper here!
Can anti-diabetes drugs be repurposed to treat cocaine addiction?
or technically,
Glucagon-like peptide-1 receptor activation in the ventral tegmental area attenuates cocaine seeking in rats.
[See Original Abstract on Pubmed]
or technically,
Glucagon-like peptide-1 receptor activation in the ventral tegmental area attenuates cocaine seeking in rats.
[See Original Abstract on Pubmed]
Authors of the study: Nicole S. Hernandez, Kelsey Y. Ige, Elizabeth G. Mietlicki-Baase, Gian Carlo Molina-Castro, Christopher A. Turner, Matthew R. Hayes, & Heath D. Schmidt
So what is this drug, and how does it work? In the last decade, the FDA approved several drugs for the treatment of Type II Diabetes. One of these drugs, Exendin-4, works by acting like a hormoneA substance produced in the body that controls or regulates the activity of certain cells or organs. Many hormones are produced by special glands and travel through the blood to reach the location in the body where they act. that is released by cells in the intestine and neuronsA nerve cell that uses electrical and chemical signals to send information to other cells including other neurons and muscles in the brainThe brain is an organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals., called glucagon-like peptide-1 (GLP-1). In the brainThe brain is an organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals., GLP-1 binds to GLP-1 receptorsA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron. and activates them, which stimulates neuronsA nerve cell that uses electrical and chemical signals to send information to other cells including other neurons and muscles that reduce food intake. Exendin-4, the drug used in Nicole’s study, also activates GLP-1 receptorsA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron. and therefore has the same effect as GLP-1 itself. GLP-1, aside from reducing food intake, also affects the brainThe brain is an organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals.'s reward system. Since drugs of abuse act on this system, Dr. Schmidt’s lab tested whether Exendin-4 would affect the rewarding properties of cocaine. Indeed, Exendin-4 decreased the amount of cocaine rats took when given free access to the drug. However, it still wasn’t clear how Exendin-4 would affect cocaine craving. Craving can be measured by determining how hard rats are willing to work to get more cocaine, which they call cocaine seeking behavior. Specifically, they tested how many times rats would press a lever that was previously paired with cocaine but was no longer. Nicole found that treating rats given Exendin-4 did not work as hard to seek out cocaine: there was a decrease in cocaine seeking. This suggested that rats did not crave cocaine as much after receiving Exendin-4. Interestingly, this was the case even when given doses of Exendin-4 that were too low to affect food intake and body weight, suggesting that this medication may be used in cocaine addicts without any adverse effects such as weight loss or changes in appetite. As such, maybe Exendin-4 could be a first step in curbing drug relapse!
Armed with this interesting finding, Nicole tried to understand where this drug might be acting in the brainThe brain is an organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals.. She thought it might be acting in the ventral tegmental area (VTA). The VTA is a region of the brainThe brain is an organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals. rich in GLP-1 receptorsA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron. and part of the brainThe brain is an organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals.’s reward system that is very active in response to cocaine. To see if Exendin-4 might be acting in the VTA to reduce cocaine seeking, she blocked GLP-1 receptorsA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron. in the VTA and repeated the experiment. When GLP-1 receptorsA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron. in the VTA were blocked, Exendin-4 no longer reduced cocaine seeking. Remember, Exendin-4 normally activates GLP-1 receptorsA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron., so this result suggests that in order for Exendin-4 to reduce cocaine seeking, it needs to be able to activate GLP-1 receptorsA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron. in the VTA. This is very strong evidence that Exendin-4 reduces cocaine seeking by activating GLP-1 receptorsA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron. in brainThe brain is an organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals. regions involved in reward.
This study uncovered a possible new use for drugs that activate GLP-1 receptorsA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron., like Exendin-4. It also opens the door to several future experiments. For example, while Nicole showed that activating GLP-1 receptorsA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron. in the VTA might reduce cocaine seeking, it is still not clear how this happens. The VTA is a region of the brainThe brain is an organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals. that produces dopamineA neurotransmitter produced by neurons in the brain that regulates movement and emotion.. DopamineA neurotransmitter produced by neurons in the brain that regulates movement and emotion. is a chemical typically released during pleasurable experiences, such as food consumption and social interactions. Cocaine and other drugs of abuse hijack this system, increasing dopamineA neurotransmitter produced by neurons in the brain that regulates movement and emotion. signalling, which promotes addiction. It is possible that GLP-1 receptorA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron. activation decreases the amount of dopamineA neurotransmitter produced by neurons in the brain that regulates movement and emotion. that is released to the rest of the brainThe brain is an organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals. , which might blunt the addictive property of cocaine. While more research is needed to support this hypothesis, Nicole’s study sheds light on a possible new use for GLP-1 receptorA molecule that binds to a chemical signal and causes a change inside a cell. For example, a receptor on the outside of a neuron can bind to a neurotransmitter released from a different neuron. activators such as Exendin-4, already on the market to treat diabetes, in the treatment of cocaine addiction.
About the brief writer: Nitsan Goldstein
Nitsan is a third year graduate student in Nick Betley’s lab. She is interested in how the brain senses the energy needs of the body and coordinates appropriate behaviors
Citations:
Warner M, Trinidad JP, Bastian BA, et al. Drugs most frequently involved in drug overdose deaths: United States, 2010–2014. National vital statistics reports; vol 65 no 10. Hyattsville, MD: National Center for Health Statistics. 2016.
Schmidt HD, Mietlicki-Baase EG, Ige KY, Maurer JJ, Reiner DJ, Zimmer DJ, et al. Glucagon-like peptide-1 receptor activation in the ventral tegmental area decreases the reinforcing efficacy of cocaine. Neuropsychopharmacology. 2016;41:1917–1928.